Unhealthy balance of the bacteria that reside in the gastrointestinal tract is one of the most important causes of chronic unwellness and disease. Virtually any condition you can think of may be related, at least in part, to an unhealthy population of bacteria in the gut. This state of imbalance, called dysbiosis, is the rule and not the exception for the average American, due in part to what we eat. The specific mix of undesirable bacteria can be vastly different from one sick person to the next. The exciting news is that a revolutionary new stool test called GutID can identify and quantify every single strain of bacteria comprising the microbiome! This provides the information needed to solve chronic health puzzles. Everyone can benefit from acting on the information this test provides.

I began to learn about the human microbiome and leaky gut syndrome more than 3 decades ago. Conventional medicine can no longer deny the importance of these influences on health even if the phrase “leaky gut syndrome” is not in favor. As of this writing there are 296 peer-reviewed articles identified by using PUBMED, the search engine of the National library of Medicine. Searching with the more accepted term, “increased intestinal permeability” reveals 16,605 published studies. Searching “Dysbiosis”, meaning unhealthy imbalances in types of normally present bacteria, reveals 25,766 studies. What’s more impressive than the numbers are the varied powerful health effects from dysbiosis and leaky gut syndrome.
It’s a bit disconcerting to find out that we are covered in bacteria! Our skin, mouth, gastrointestinal tract, genitourinary tract, lungs, and eyes all are home to bacteria. Even breast milk has bacteria!
The gastrointestinal tract, primarily the colon, houses the most bacteria. The average person hosts several hundred to more than 1000 different types of bacteria, weighing a total of several pounds. These 10-100 trillion bacteria outnumber human cells. It makes sense that most of the immune system is clustered around the gastrointestinal tract to protect us from these bacteria. If the gut bacteria had ready access to the blood stream, we would die. That process is called sepsis or blood poisoning. Leaky gut syndrome is a milder, extremely common, version of sepsis and contributes to adverse effects throughout the entire body – from the liver to the heart to the sexual organs to the brain – the whole body is negatively affected.
The microbiome functions as a vital organ, with an extremely broad metabolic capacity that surpasses even that of the liver. Each bacterial strain has its own distinct characteristics and metabolic influences, and together, in a healthy state of balance, these microbes can be thought of as a, diverse thriving garden, where a small number of weeds is fine. However, too many weeds cause trouble. Certain bacteria are especially beneficial—they support digestion, synthesize important nutrients, regulate and educate our immune system – inhibiting allergy and inflammation and infections, help manage appetite, improve blood sugar and cholesterol levels, regulate metabolism and reduce the risk of obesity and muscle loss, and promote mental well-being. Remarkably, some may even contribute to breaking down microplastics that we ingest!
The short-chain fatty acids (SCFAs) these bacteria produce from feeding on fermentable carbohydrates that we eat, offer a range of health benefits, for gut and overall health. SCFAs enhance mineral absorption and play a role in maintaining a healthy intestinal ecosystem, limiting overgrowth of unfriendly organisms. SCFAs are the main fuel for colon cells but also have systemic beneficial effects on appetite, body fat, muscle, heart, brain, liver, immune system, endocrine system, bone, and more.
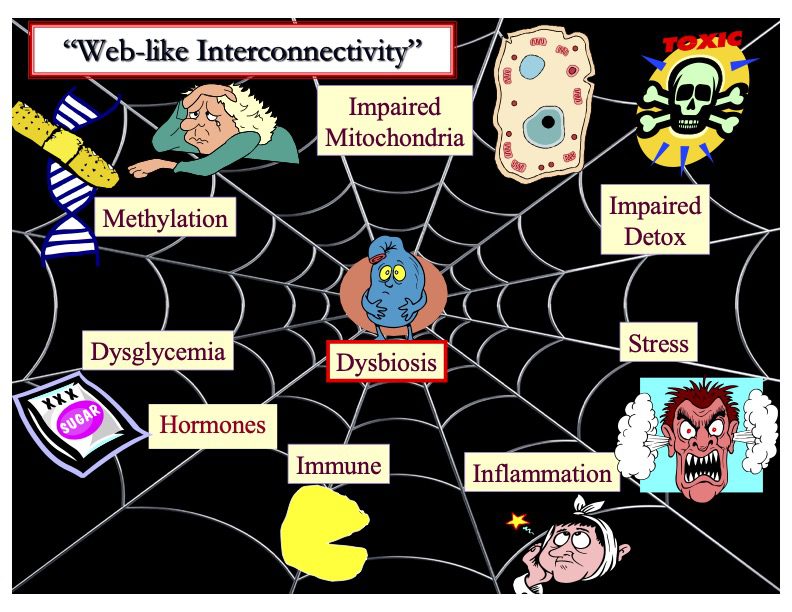
When “weeds”—or harmful bacteria—overgrow in the gut without enough beneficial microbes to keep them in check, the consequences can be severe. While digestive issues like gas, bloating, diarrhea, constipation, and abdominal pain are common signs, the impact of this imbalance, known as dysbiosis, reaches far beyond the digestive tract. Dysbiosis has been linked to the onset and progression of obesity, fatty liver disease, diabetes, metabolic syndrome, abnormal cholesterol levels, cardiovascular disease, chronic kidney disease, sarcopenia, and even certain cancers. It can also disrupt immune function, increasing susceptibility to allergies, autoimmune conditions, and chronic inflammation.
A disrupted gut microbiota can compromise the gut barrier, leading to what’s known as “leaky gut.” This allows bacterial toxins such as lipopolysaccharides (LPS) to enter the bloodstream, triggering widespread inflammation throughout the body.
Chronic inflammation has long been recognized as a key driver of cardiovascular disease and is a common thread in all age-related diseases. The immune system plays a central role in inflammation—and remarkably, the majority of our immune cells reside in the gastrointestinal tract. Every day, your gut’s immune system is exposed to more potential threats from bacteria, food components, and toxins than your blood-borne immune system encounters in a lifetime! It’s no wonder the saying goes, “death begins in the colon.” Given this, dysbiosis and leaky gut syndrome—resulting in endotoxemia (the leakage of bacterial toxins into the blood)—should be considered prime suspects in any chronic disease.
The altered metabolic function and structural damage from the inflammatory process creates a variety of unpleasant symptoms and contributes to food reactions, skin problems, joint pain, high blood pressure, dyslipidemia, cardiovascular disease, kidney disease, liver disease, chronic fatigue syndrome, hypothyroidism, low progesterone and testosterone, polycystic ovary syndrome (PCOS), infertility and miscarriage, erectile dysfunction, increased susceptibility to infections, and more! Additionally, dysbiosis has been linked to neurological and mental health issues, in part because of blood-brain barrier disruption (leaky brain) from endotoxemia (LPS or bacterial toxins leaking into the blood stream). Some of the resulting conditions include anxiety, depression, eating disorders, alcoholism, Parkinson’s and Alzheimer’s diseases, autism, attention-deficit/ hyperactivity disorder (ADHD), and schizophrenia. Not to say that dysbiosis and leaky gut syndrome are the only causes of these conditions but their major influence needs to be considered and investigated.
More than half of the metabolites (small molecules produced in the process of metabolism) in your bloodstream are produced by gut bacteria! Obviously, the composition of the microbiome is critical to good health. The microbiome can be altered significantly within a few days if any of a number of conditions change.
What influences the make-up of the bacteria in the microbiome? Genetics play somewhat of a role. The microbiome of our mothers, whether we were delivered vaginally or by c-section, and whether breast or formula fed are early influences. Age, diet, fasting, exercise, stress, sleep, nutritional supplements, medications (especially antibiotics), toxins (including refined, ultra-processed foods and additives), electromagnetic radiation, temperature, environment, and pets impact the microbiome. Maldigestion from any cause, including acid-suppressing medication, and altered intestinal transit time (diarrhea or constipation), modify the intestinal flora composition. Illness and disease can become locked in a vicious cycle with dysbiosis. For example, certain bacteria produce metabolites that damage the kidneys. Altered kidney function, in turn, leads to more dysbiosis. It is worth noting that kidney function naturally declines with age.
There is a predictable unhealthy change in the microbiome with age, which leads to the conclusion that rebalancing the flora may be an important anti-aging strategy.
A number of natural supplements and some medications exert their effects, in part, by interacting with the microbiome. For example, berberine, which improves insulin sensitivity, blood sugar, lipids, and reduces bodyfat, kills some unfriendly bacteria while fostering the growth of more beneficial organisms. This leads to an increase in SCFAs and the hormone GLP-1, which is a target of popular weight-loss drugs.
Some drugs will not work as well or be tolerated as well if they are passing through a dysbiotic gastrointestinal tract on the way to being absorbed. Importantly, medications can be a significant contributor to dysbiosis. This is a big issue in the elderly who are on multiple drugs. The unhealthy changes that occur in the body from the medication-induced dysbiosis are given a name (a diagnosis) and then are “treated” with another medication – which may cause further dysbiosis! For example, proton pump inhibitor drugs shut off stomach acid, which is necessary for digestion. These drugs, commonly used for symptoms of gastroesophageal reflux, result in undigested food becoming available to spur the growth of unfriendly intestinal bacteria and thereby cause dysbiosis. These drugs have been associated with increased depression, among many other conditions. Such patients may be prescribed a selective serotonin reuptake inhibitor drug, which causes its own bacterial imbalances!
A good way to gain further understanding of the importance and wide-ranging impact of the microbiome is to learn about the things that have been affected by fecal microbial transplant (FMT). FMT is a treatment that introduces the microbiome from a healthy individual into the gastrointestinal tract of an unhealthy person in order to reestablish a normal microbiome. The first condition approved for this procedure was recurrent intestinal Clostridioides difficile (C. difficile) infection.
Beyond solving a difficult-to-treat life-threatening infection (C. difficile), growing research supports the potential of FMT in other conditions. Inflammatory bowel diseases like ulcerative colitis and Crohn’s disease, as well as irritable bowel syndrome (IBS) have been found to benefit. In early studies, FMT has shown promise in improving gastrointestinal and behavioral symptoms in children with autism, and has demonstrated some metabolic benefits, such as better insulin sensitivity, in individuals with obesity or metabolic syndrome. Additionally, emerging research suggests possible benefit in neurological conditions like Parkinson’s disease, multiple sclerosis, and chronic fatigue syndrome, though evidence remains limited in these areas.
An even greater understanding of the powerful influence of the microbiome results from an examination of studies that have been done on animals. Some experiments have transplanted human microbiomes and found striking results.
- Obesity: Healthy mice receiving FMT from obese donors gained more weight and developed insulin resistance.
- Transplanting bacteria from lean animals to obese animals reduces inflammation, improves glucose and insulin metabolism, and results in weight loss!
- Immune Modulation: FMT has demonstrated the ability to regulate immune responses, potentially benefiting animals with autoimmune or inflammatory conditions
- Non-Alcoholic Fatty Liver Disease (NAFLD) models: FMT improved liver function and reduced fat accumulation.
- Inflammatory Bowel Disease: A Fasting-Mimicking Diet led to improvement in an animal model of inflammatory bowel disease, and FMT from these treated animals to untreated diseased animals resulted in significant benefits.
- Behavioral and neurological effects: FMT modulates animal behavior, with notable improvements in mood, cognition, pain response, and motor function
- Autism models (mice): FMT improved social behavior, reduced repetitive behaviors, and normalized microbiome composition.
- Depression & anxiety models: Healthy mice receiving FMT from depressed donors showed depressive-like behaviors; healthy FMT reversed some of these effects.
- Parkinson’s models: Transferring feces from Parkinson’s patients to mice induced motor deficits; FMT from healthy donors improved symptoms.
- Hypertension: FMT from rats with normal blood pressure to rats with high blood pressure resulted in reduction of blood pressure in the recipient animals.
- FMT from humans with high blood pressure to germ-free mice caused an increase in blood pressure in the mice!
- Cancer: FMT from mice with colon cancer to healthy mice produced precancerous changes.
- Mice with colorectal cancer given FMT from healthy mice experienced improvement of their microbiome, enhanced cancer-killing immune response, reduced cancer progression, and prolonged survival!
- Aging Reversal!: In mice, FMT from young donors to aged recipients has reversed age-related changes in the gut, brain, and retina, reducing inflammation and improving tissue function!
Don’t think you have to resort to FMT to see benefit. Targeted diet and supplements are first-line therapeutic tools in reshaping the microbiome.
Dietary modulation of the microbiome to alter health is illustrated by an animal study that found feeding a high-fat diet led to the development of leaky gut syndrome, insulin resistance, systemic inflammation, and obesity. When the experiment was repeated with animals that had their intestinal bacteria eliminated through sterilization, these harmful effects did not appear despite the same high-fat diet.
In a further variation of the experiment, animals were given a high-fat diet along with a prebiotic—a substance that feeds beneficial gut bacteria like bifidobacteria. This combination prevented the negative metabolic consequences usually associated with a high-fat diet.
By this point, if you can’t appreciate the importance of having your microbiome meticulously and accurately analyzed, dysbiosis may be impairing your judgement!
GutID represents a revolutionary breakthrough in microbiome assessment. Other functional medicine labs offer microbiome tests but comparing them is like comparing the view with a magnifying glass with that of a microscope. These other tests are extremely limited in the number of bacteria the technology is able to identify. GutID identifies 100% of the bacteria in a stool specimen! Even previously unknown organisms are identified with this test! GutID uses next-generation DNA sequencing (looking at the 16S, ITS, 23S genes) to analyze your stool sample. Unlike most tests that only identify bacteria at a broad level, GutID goes deeper—detecting every bacterial strain in your gut. Even previously unknown organisms are identified with this test! This is possible because of the proprietary Titan-1™ platform, which doesn’t rely on limited reference databases. With GutID, you get the most complete and accurate picture of your gut health available today.
With results of the GutID, therapeutic interventions can be tailored to resolve dysbiosis and create a healthy state of microbial balance. Of course, not only may gastrointestinal symptoms be improved, but all types of systemic conditions are impacted. For example, if cardiovascular risk is a concern, I will be paying particular attention to levels of bacteria known to produce TMA from dietary or supplemental carnitine and phosphatidylcholine. TMA gets absorbed and converted by the liver to TMAO, which damages the cardiovascular system and much more. TMAO is linked to a variety of health conditions, including hypertension, chronic kidney disease, osteoporosis, colorectal cancer, neuropsychiatric disorders, autism spectrum disorders, mild cognitive impairment in patients with type 2 diabetes, and increased all-cause mortality in individuals with nonalcoholic fatty liver disease (NAFLD), among others.
The GutID report provides levels of your bacteria in association with different health conditions. You can see how your levels compare with healthy ranges for the following conditions:
- Irritable Bowel Syndrome (IBS)
- Small Intestinal Bacterial Overgrowth
- Inflammatory Bowel Disease
- Bile Acids Metabolism
- Obesity
- Type 2 Diabetes
- Non-Alcoholic Fatty Liver Disease
- Mood Disorders
- Alzheimer’s Disease Risk
- Parkinson’s Disease Risk
- Hypertension
- Atherosclerosis
- Trimethylamine (TMA) Production
- Atherosclerosis
- Lipopolysaccharide (LPS) Production
- Mucosa Protection
- Short-Chain Fatty Acids (SCFAs) Production
- Histamine Production
- Eczema & Atopic Dermatitis
- FODMAP Fermentation
- Indole Production
- Vitamin B Production
- Probiotics
The comprehensive GutID report offers actionable, specific recommendations to enhance your microbiome. Therapeutic foods to eat and those to reduce, prebiotics, polyphenols, targeted strains of probiotics, and other supplements are among the personalized recommendations.
Click for a sample GutID report
Click to learn more about and to order GutID