Have you been tested for the condition that may stand between you and a healthy future?
For over two decades I have been excoriated by conventional medicine for evaluating and treating patients for “leaky gut syndrome”. Thanks to a tsunami of published research, there is no scientific basis for denying this condition any longer.
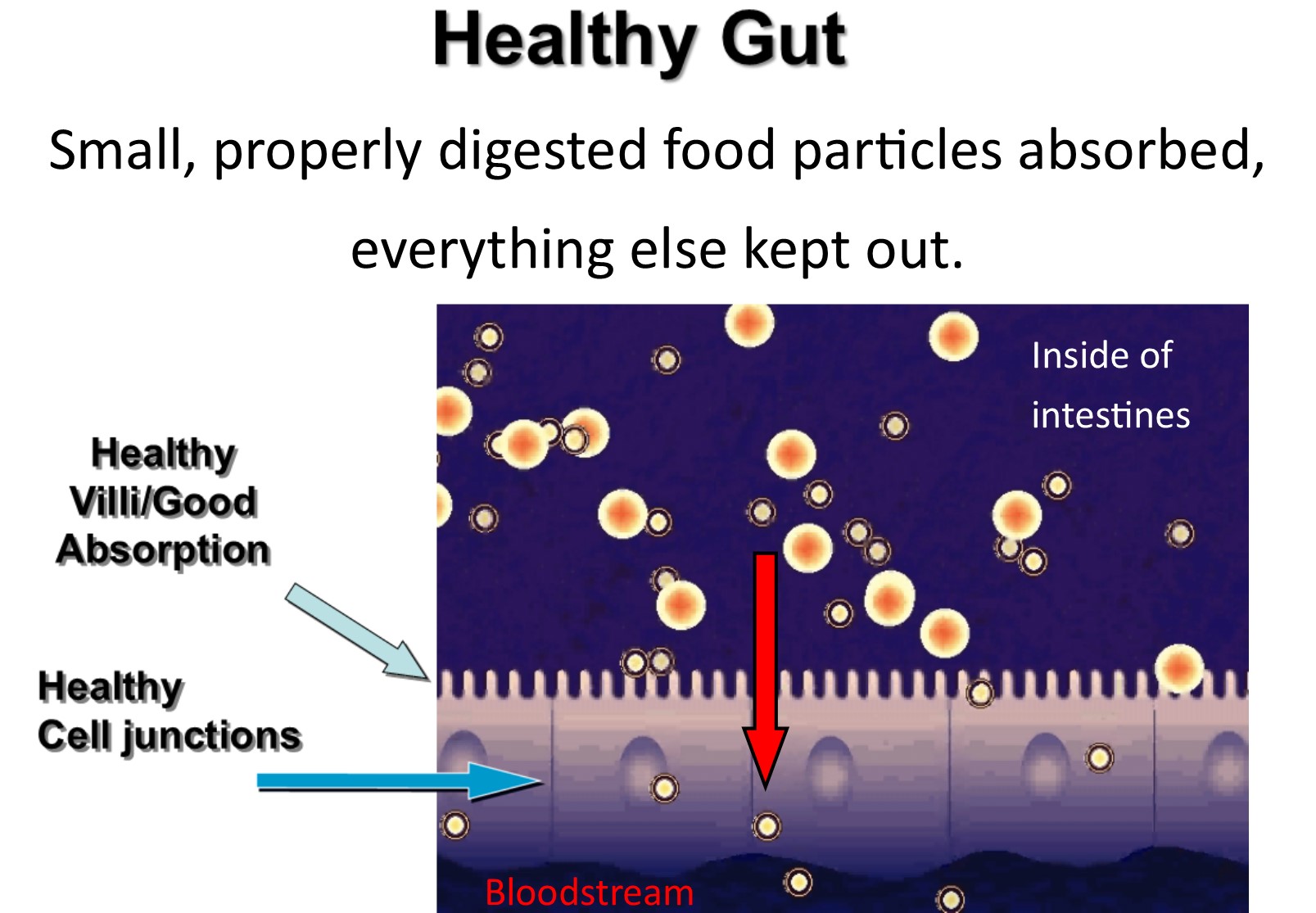
The single layer of cells that lines the intestinal tract has to perform two somewhat opposite tasks: let things into your body and keep things out of your body. Nutrients from food need to be absorbed into the bloodstream. That is, properly digested food particles need to be absorbed into the bloodstream. Large, incompletely digested food particles, however, should not pass into the bloodstream. Large particles sort of resemble organisms and are perceived by the immune system as a threat. The other thing that needs to be kept out of the bloodstream is microbes: bacteria, yeast, viruses, and parasites.
In a healthy state, only small amounts of undigested food particles and microbes pass through the cells that line the intestinal tract. The intestines are home to a hundred trillion bacteria. If these bacteria were free to cross your intestinal barrier you wouldn’t last very long. Septicemia is the sometimes fatal condition of bacterial infection in the blood.
The body has many ways to protect itself from the danger that resides in the intestinal tract. The most important of these are the physical intestinal barrier and the immune system. It makes sense that most of the immune system is clustered around the intestinal tract. If you have a health problem related to the immune system, chances are the intestinal tract is involved. The two categories of potential instigators I think of in this regard are microbes and foods. The destructive effects of food reactions and “bad microbes” are magnified by an increase in intestinal permeability, also known as leaky gut syndrome.
From autism to psoriasis, from muscle loss to schizophrenia, and from asthma to arthritis, leaky gut syndrome can be a major factor. Just about any symptom may be the result of this condition. Leaky gut syndrome has been identified in patients with Chronic fatigue syndrome, and its successful treatment has relieved symptoms. The first effect I learned of in connection with leaky gut syndrome was autointoxication. If a person embarks upon a detoxification program to clear stored toxins from the body but doesn’t address the source of exposure of the toxins, any benefit will be short-lived. Therefore, healing a leaky gut is often an important strategy for optimal detoxification.
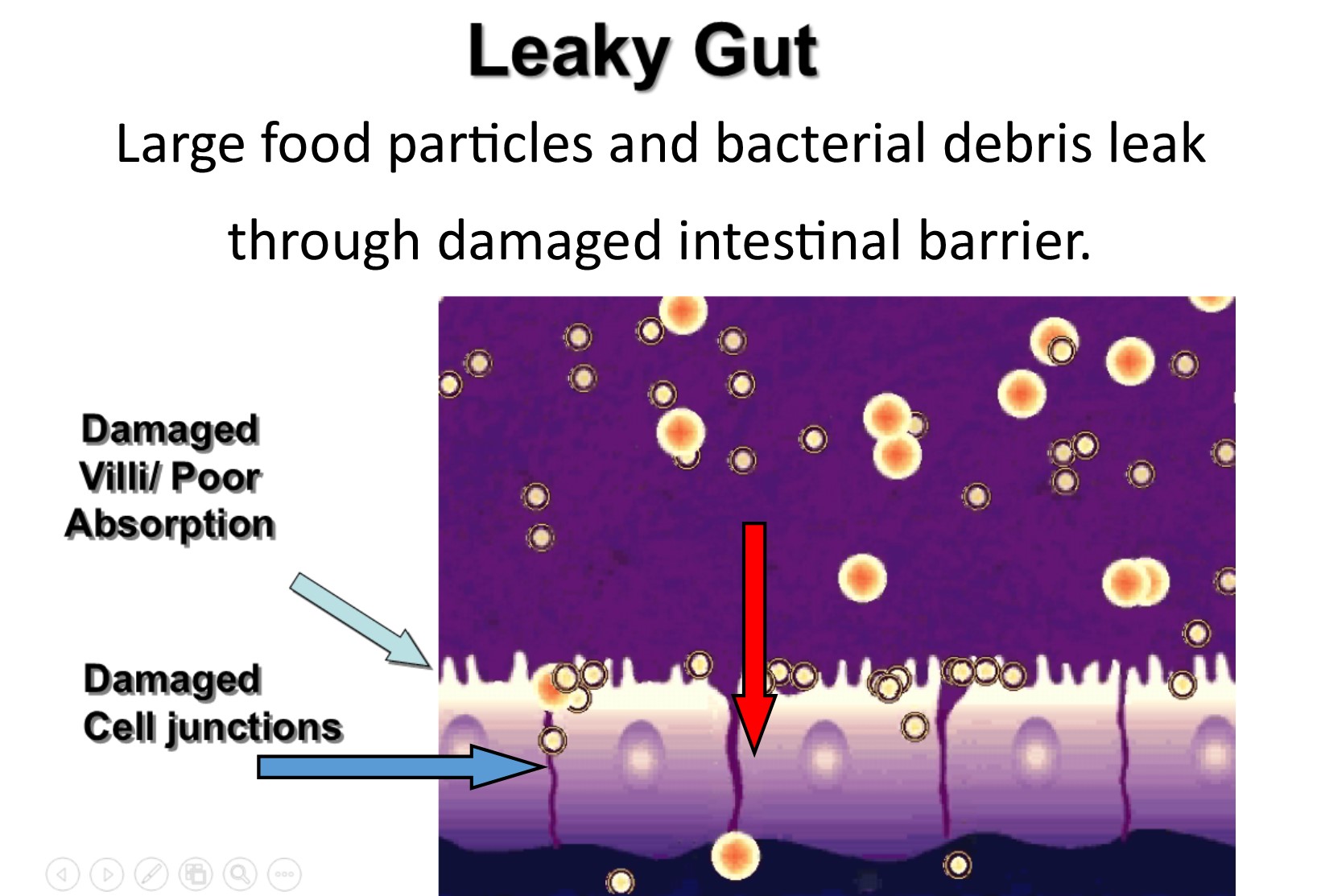
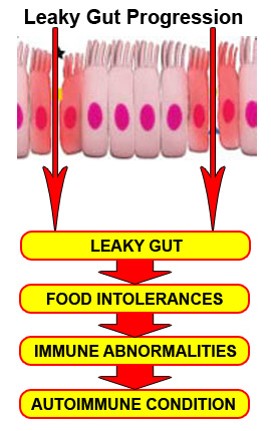
A more sophisticated mechanism of damage produced by leaky gut syndrome involves inflammation and autoimmunity. When large particles of food or bacterial fragments pass through a leaky gut, the immune system is activated. The resulting inflammation can affect the liver, kidneys, ovaries, thyroid, skin, joints, brain…virtually any and every organ and tissue. Inflammation produces insulin resistance and all of its damaging health effects including obesity, diabetes, high blood pressure and cholesterol, fatty liver, certain cancers, polycystic ovary syndrome, and much more. (For more on this: “Reversing the Number 1 cause of illness, obesity, and accelerated aging“). An increase in the number and severity of food immune reactions is a predictable result of leaky gut syndrome. A vicious cycle of food sensitivity-leaky gut-food sensitivity reactions can develop. Autoimmunity can eventually follow. Probably in excess of 70 million Americans have an autoimmune disease. When you consider that heart disease and Alzheimer’s disease have autoimmune characteristics, autoimmunity may be our number 1 killer.
How do you know if you have leaky gut syndrome? You can’t simply go by symptoms. Although leaky gut syndrome may be an important factor in virtually any health condition, there are few symptoms where leaky gut syndrome is always present. Depression? Leaky gut syndrome may or may not be a factor. Migraines? Infertility? Hypothyroidism? Leaky gut syndrome may or may not be present. The best way to know the status of your intestinal barrier is with lab testing. The best test I know of is by Cyrex Labs. It’s called Intestinal Antigenic Permeability Screen. I think it is a good idea to “Test, treat, retest.” Why treat a condition you don’t have? Also, if you don’t get a baseline test you won’t be able to track your progress. You can’t rely on symptoms alone to determine if you have a leaky gut…or when a leaky gut has been healed. For example, in a study of Crohn’s disease patients who were in remission (free of symptoms), a test of intestinal permeability or leaky gut was performed. Even though they were symptom-free, some of these people had evidence of having leaky gut syndrome. One hundred percent of these individuals with leaky gut syndrome had a flare-up of Crohn’s disease within the next six months.
Once leaky gut syndrome is identified, the possible contributing factors should be investigated. A few of the many factors that play a role include food sensitivities, stress, dysbiosis or intestinal bacterial imbalances, and nutrient deficiencies. Certain medications, including antibiotics, steroids and non-steroidal anti-inflammatory drugs, may cause leaky gut syndrome. How ironic is that? People often are treated for conditions that can be caused by leaky gut syndrome with a medication that causes leaky gut syndrome! Your pain and inflammation may be temporarily reduced while you take these drugs but your health is actually deteriorating. I believe medications are often an important cause of these chronic health conditions.
Alcohol is an important cause of leaky gut. Much of the liver damage that results from excessive alcohol intake is not directly from the alcohol but secondary to leaky gut syndrome. The leaky gut caused by alcohol causes increased passage of intestinal bacterial debris into the bloodstream and the first stop is the liver. Inflammatory chemicals resulting from leaky gut syndrome can reach every organ. The brain inflammation from leaky gut syndrome contributes to depression and to alcohol craving. Here we have another vicious cycle:
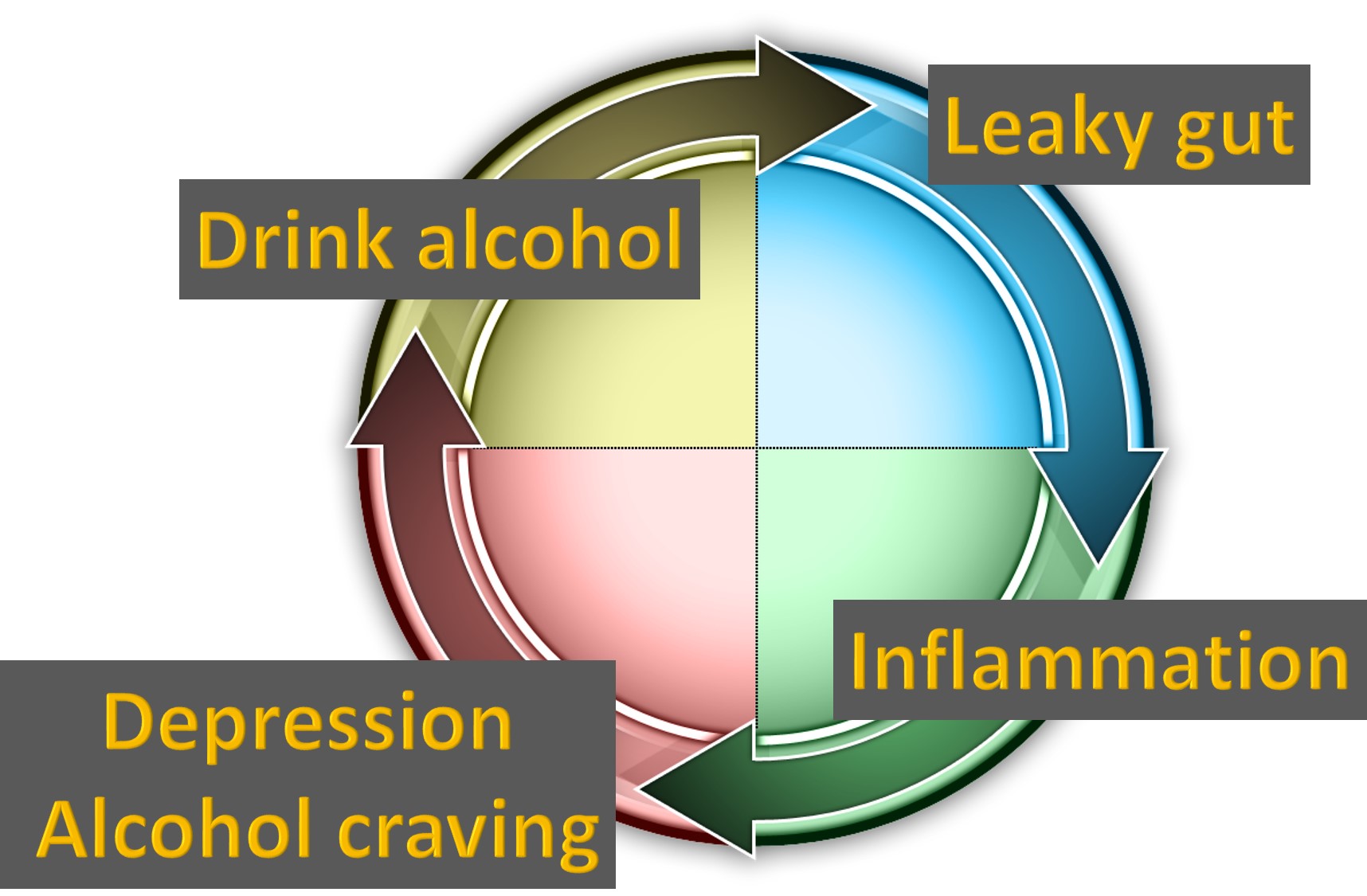
It would appear that strategies to heal leaky gut should be part of any alcohol-dependence recovery program. Experimental studies have found melatonin, betaine, and N-acetylcysteine to help protect against leaky gut syndrome induced by alcohol.
A thorough evaluation of the patient’s diet, lifestyle, rest, exercise, stress, supplements, and medications should be undertaken. Laboratory testing to check for potential inciting food reactions should be done. A number of other lab tests are often important, including a comprehensive digestive stool analysis or gastrointestinal function profile to learn about the make-up of the intestinal flora and much more. These tests identify intestinal inflammation and measure the short chain fatty acids, which are an important fuel source to keep intestinal cells healthy.
In addition to a nutrient-dense whole foods diet that eliminates processed foods, a number of supplements can accelerate healing of a leaky gut.
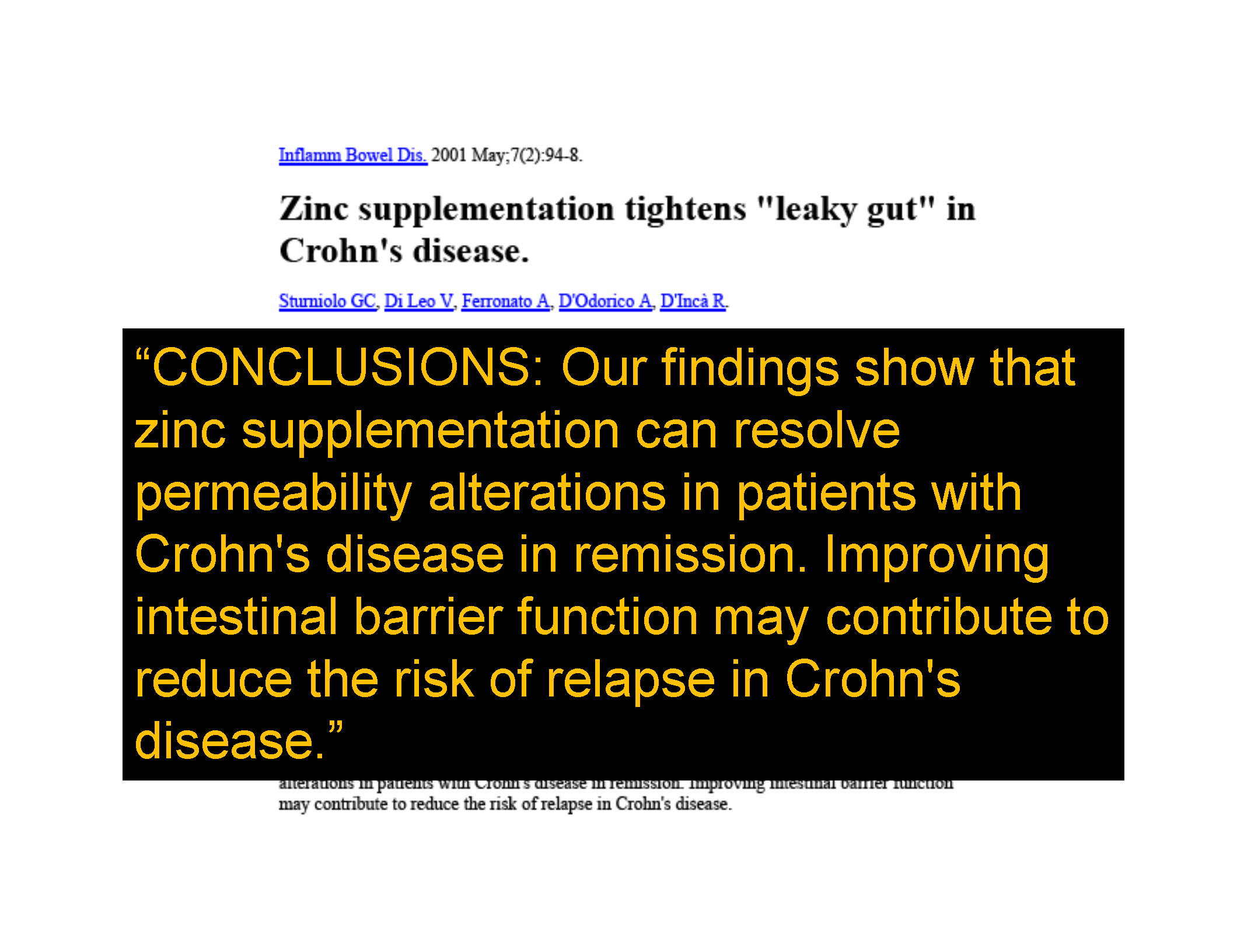
Individual nutrients such as zinc are important. However, a comprehensive approach is likely to produce better results. Glutagenics and GI Sustain were formulated specifically to help resolve leaky gut syndrome.
To conclude, ask your doctor about getting an Intestinal Antigenic Permeability Screen if you want to know if leaky gut syndrome is affecting your health and wellbeing. It could be the most important test you ever take.